In all my years of treating clients with therapeutic massage, until recently I had never encountered someone suffering from trigeminal neuralgia. Client S (as she will be referred to) presented with debilitating pain in her scalp,  forehead, temple region, and jaw. She told me she had been diagnosed with Trigeminal Neuralgia and was seeking help from therapeutic massage. Since this was something I had not dealt with in the past we attempted a very short therapeutic treatment for her first session. But I immediately did some research and learned a good deal about this terrible condition and wanted to post something for those of you who may be suffering and looking for an alternative means of relief.
forehead, temple region, and jaw. She told me she had been diagnosed with Trigeminal Neuralgia and was seeking help from therapeutic massage. Since this was something I had not dealt with in the past we attempted a very short therapeutic treatment for her first session. But I immediately did some research and learned a good deal about this terrible condition and wanted to post something for those of you who may be suffering and looking for an alternative means of relief.
I will be posting excerpts from two different articles I discovered online about Trigeminal Neuralgia and Massage Therapy below, crediting the authors accordingly. Client S has already told me that she has had several days without any pain and is very thankful for the treatments we have begun.
The first article comes from Linda LePelley, RN, NMT , written May 1, 2016. She writes:
“TN usually occurs when the myelin sheath of the trigeminal nerve has been worn away, sometimes due to a blood vessel causing compression to the nerve, or if the patient has Multiple Sclerosis, a disease which attacks the myelin sheath. Sometimes TN can be brought on by an arteriovenous malformation or a tumor. Trauma, dental work, and strokes affecting the nerve can also trigger TN. The trigeminal nerve consists of three branches, which service the face and up into the scalp. Any branch, and more than one, can be affected. Occasionally, it can occur bilaterally.
When diagnosed, TN is classified as one of two types, which The National Institute of Neurological Disorders and Stroke describes as follows: The typical or “classic” form of the disorder (called “Type 1” or TN1) causes extreme, sporadic, sudden burning or shock-like facial pain that lasts anywhere from a few seconds to as long as two minutes per episode. These attacks can occur in quick succession, in volleys lasting as long as two hours. The “atypical” form of the disorder (called “Type 2” or TN2), is characterized by constant aching, burning, stabbing pain of somewhat lower intensity than Type 1. Both forms of pain may occur in the same person, sometimes at the same time. The intensity of pain can be physically and mentally incapacitating.
TN is serious in that the pain is debilitating. According to the NIH, the incidence of new cases is about 12 per 100,000 people a year, and is more frequently found in women. Current treatment for TN begins with anticonvulsant medications, and tricyclic antidepressants are prescribed for pain relief. TN is not believed to be related to depression or psychological factors, but analgesics are generally ineffective.
TN is a progressive condition, and if medications lose their effect over time, there are more invasive treatments available for pain relief. These include injections and several different types of surgery, all which involve the risk of unpleasant side effects. The NIH handout for TN states, “Some individuals manage trigeminal neuralgia using complementary techniques, usually in combination with drug treatment.” Although they list low-impact exercise, yoga, and visualization among other approaches, there is no mention of massage therapy. In my limited experience, massage therapy for TN has relieved everyone who has attempted it. From what I understand of this condition, it progresses over time. As the tissues become more compressed, the pain becomes more intense. If heat and massage can soften, mobilize, and relieve pain elsewhere in the body as it does, it can certainly relieve at least some of those cases of TN. It only makes sense to try therapeutic massage before administering drugs or performing surgeries.”
The next article is from Michael Dixon on December 22, 2017. Mike Dixon has practiced massage therapy for more than 30 years. He is an educator, and an international presenter in massage therapy continuing education (Arthrokinetic Therapy).
“According to the Mayo Clinic, trigeminal neuralgia is one of the most painful afflictions known to medical practice. Trigeminal neuralgia (TN) is a disorder of the fifth cranial (trigeminal) nerve. Here I’d like to share my 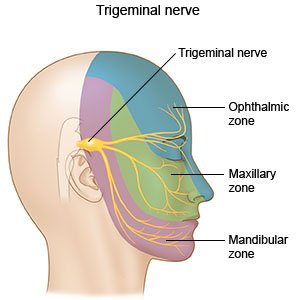 experience treating patients with TN. A few simple treatment procedures will be discussed, and I believe they are worth a try for therapists to see if they also have positive effects in treating this nerve pain.
experience treating patients with TN. A few simple treatment procedures will be discussed, and I believe they are worth a try for therapists to see if they also have positive effects in treating this nerve pain.
The typical or “classic” form of the disorder (called TN1) causes extreme, sporadic, sudden burning or shock-like pain in the areas of the face where the branches of the nerve are distributed – lips, eyes, nose, scalp, forehead, upper jaw and lower jaw. The pain episodes last from a few seconds to as long as two minutes. These attacks can occur in quick succession or in volleys lasting as long as two hours.
The “atypical” form of the disorder (called TN2), is characterized by constant aching, burning, stabbing pain of somewhat lower intensity than TN1.
Both forms of pain may occur in the same person, sometimes at the same time.
The treatment procedure I use to treat TN is very simple. It involves stretching the three branches of the trigeminal nerve on the patients’ face. This may have a positive effect by reducing the swelling caused by a build-up of edema in the nerve.
Stretching nerves – whether it is the trigeminal nerve, or the greater or lesser occipital nerve – causes a reflex effect allowing edema to exit the problematic nerve. This reduction of edema decreases the swelling of the nerve and improves its blood flow – resulting in improved function and reduced nerve pain. Improving blood flow is the key to allowing the nerve to start to heal and normalize.
In short, stretching procedures can and may result in less pain and/or a resolution of the dysfunction of the TN or any nerve that has a build-up of edema due to stress – whether mechanical, chemical or otherwise. This is the theory upon which I based the treatment procedure for patients with TN.
So, the question is: why do nerves swell with edema, become dysfunctional, and often generate nerve pain?
The answer is: stress to the nerve. When a nerve is stressed, it produces macromolecules known as proteoglycans. These long chain proteins can absorb up to 50 times their weight in water molecules thus causing a physical swelling of the nerve. The proteoglycans are like tiny sponges inside the nerve.
Why do the nerves produce proteoglycans?
The physiological response to a nerve being injured or stressed is to swell with these water molecules that attach themselves to the proteoglycans. By stretching the affected nerve, we can reduce the swelling by allowing some of the water molecules to exit through the elastic properties of the nerves.